Patient Education
We want all of our patients to be informed decision makers and fully understand any health issues they face.
Explore “Medical Mondays” on Instagram!
Common Concerns
Dr. Gunn is a board-certified dermatologist. She has over 13 years of experience purely diagnosing and treating skin conditions. We treat all skin ailments and growths including acne, rosacea, skin cancer, psoriasis, eczema, cysts, scars, and many more.
Acne
Acne is the most frequent skin condition in the United States. It is characterized by pimples that appear on the face, back, and chest. Every year, about 80% of adolescents have acne, and about 5% of adults experience acne.
-
Acne is made up of two types of blemishes:
Whiteheads/Blackheads, also known as comedones, are non-inflammatory and appear more on the face and shoulders. As long as they remain uninfected, they are unlikely to lead to scarring.
Red Pustules or Papules are inflamed pores that fill with pus. These can lead to scarring.
In normal skin, oil glands under the skin, known as sebaceous glands, produce an oily substance called sebum. The sebum moves from the bottom to the top of each hair follicle and then spills out onto the skin's surface, taking with it sloughed-off skin cells. With acne, the structure through which the sebum flows gets plugged up. This blockage traps sebum and sloughed-off cells below the skin, preventing them from being released onto the skin’s surface. If the pores opening is fully blocked, this produces a whitehead. If the pores opening is open, this produces blackheads. When either a whitehead or blackhead becomes inflamed, they can become red pustules or papules.
It is important for patients not to pick or scratch at individual lesions because it can make them inflamed and lead to long-term scarring.
-
Treating acne is a relatively slow process; there is no overnight remedy. Some treatments include:
Benzoyl Peroxide- Used in mild acne cases, benzoyl peroxide reduces the hair follicles' blockages.
Oral and Topical Antibiotics- Used to treat any infection in the pores.
Hormonal Treatments- Can be used for adult women with hormonally induced acne.
Tretinoin- A derivative of Vitamin A, tretinoin helps unplug the blocked-up material in whiteheads/blackheads. It has become a mainstay in the treatment of acne.
Extraction- Removal of whiteheads and blackheads using a small metal instrument centered on the comedone and pushed down, extruding the blocked pore.
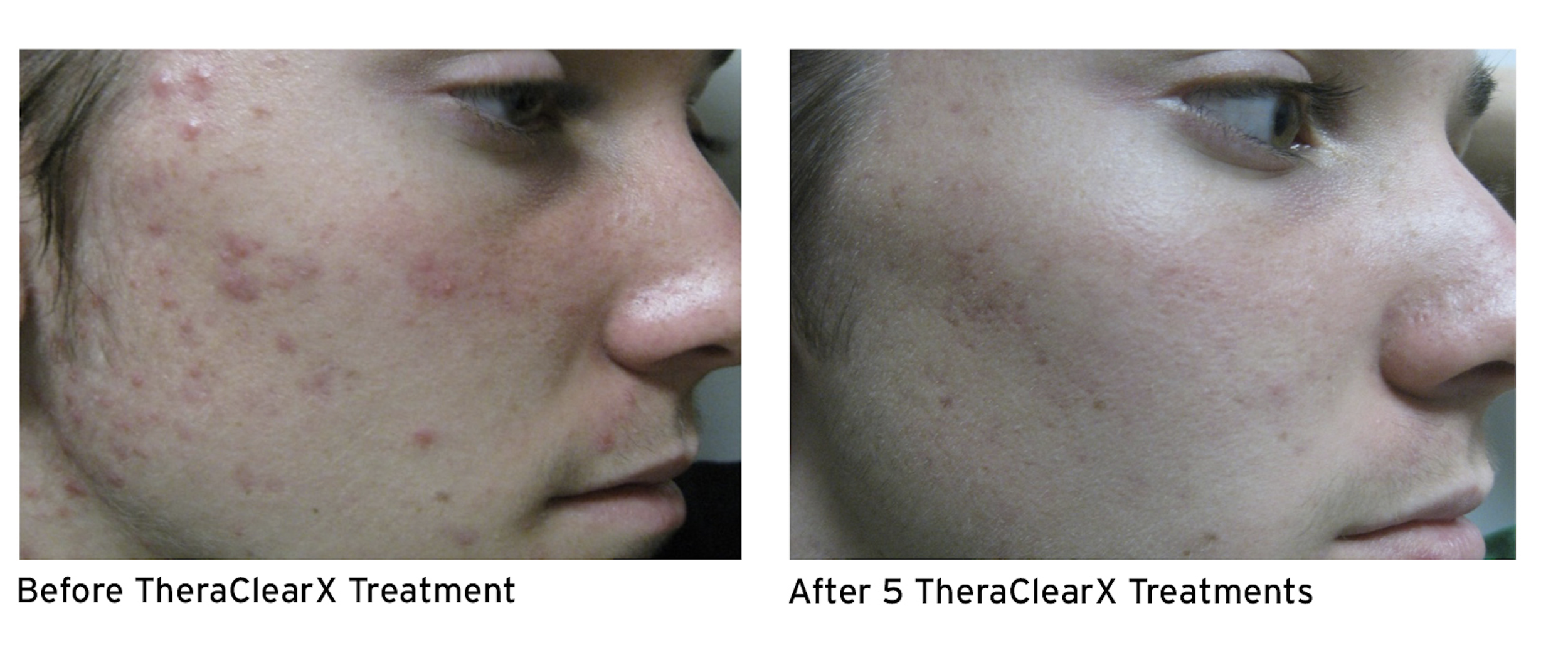
TheraClearX
TheraClearX is a noninvasive, in-office acne treatment system. Engineered and FDA-cleared for the treatment of mild-to-moderate acne including comedonal, pustular, and inflammatory acne vulgaris.
-
Combines vacuum + broadband light technology delivered through a liquid-cooled, handheld delivery system
Comfortable treatment with no downtime.
Visible improvement can be seen as early as treatment 2.
Treatment can be done on the face, back, and chest.
-
$250 per treatment and we typically recommend 6 treatments spaced out every 1-2 weeks for best results.
Wrinkles
Wrinkles can be treated with neuromodulator injections. These injections are the #1 non-surgical cosmetic procedure in North America. At Gunn Deramtology we use Botox, Dysport, Jeuveau, and Xeomin. This powerhouse anti-aging treatment can smooth frown lines, forehead wrinkles, crows feet and more, resulting in a smoother, less tired or angry-looking face.
-
Neuromodulators are approved by the FDA to temporarily relax specific muscles by blocking the nerve impulses. As the treated muscles relax, wrinkles and lines created by their movement gradually fade, and sometimes even disappear completely resulting in smoother, less wrinkled skin. The younger a person starts using neuromodulators, the smoother their face will appear as they age. Regularly scheduled appointments can actually prevent wrinkles including common forehead wrinkles and under-eye wrinkles.
The most popular treatment areas for neuromodulators include forehead lines, frown lines, bunny lines, crow’s feet, slimming of the jaw, dimpled chin, gummy smile, lip lines and so much more. Neuromodulator injections are extremely safe when administered by an experienced practitioner with extensive knowledge of facial anatomy.
-
Botox, Dysport, Jeuveau, and Xeomin are muscle relaxers that temporarily relax specific muscles by blocking the nerve impulses to those muscles. As the treated muscles relax, wrinkles and lines created by their contraction gradually fade and sometimes even disappear completely.
XTRAC
FOR PSORIASIS & VITILIGO
XTRAC is the only FDA-cleared, clinically proven excimer laser that gets skin clear of psoriasis—and it works fast, with many patients seeing significant improvement and long-lasting remissions. Because XTRAC delivers a highly targeted, therapeutic beam of UVB light only to areas of the skin affected by psoriasis, healthy skin surrounding the lesions stays that way.
-
XTRAC clears the symptoms, prolongs the remission and returns skin to a clinically healthy state in record time. All of which means XTRAC delivers consistently predictable results so patients experience more good days of living than bad.
Effective treatment—symptoms reduced generally in 10-12 treatment sessions
Long-lasting relief—typically several months free of symptoms"
Simple, painless treatment—sessions are very short
Relief without messy creams and daily skin care regimen
Covered by most major insurance companies, available by Rx
-
XTRAC treatments can minimize and, in many cases, even eliminate Vitiligo depigmented patches. The XTRAC [308 nm] excimer laser delivers a targeted beam of UVB light and only the areas of skin affected by Vitiligo receive the laser energy.
Though the laser spot size measures only 18mm x 18mm, due to rapid exposure times, relatively large, discrete areas can be treated in just five to 10 minutes, which is much quicker than the duration of conventional phototherapy light sessions. And most importantly, XTRAC treatments achieve complete response rates faster in a higher proportion of patients.
Birthmarks
Birthmarks are abnormal skin colorations in spots that are either present at birth or appear shortly thereafter. They can be flat or slightly raised from the skin. They can be any number of colors, including red, brown, black, tan, pink, white, or purple. Birthmarks are generally harmless. There are two major categories of birthmarks: pigmented birthmarks and red birthmarks.
-
Pigmented Birthmarks can grow anywhere on the skin and at any time. They are usually black, brown, or skin-colored and appear singly or in groups. They can be moles (congenital nevi) present at birth, Mongolian spots, which look like bluish bruises and appear more frequently on people with dark skin, or café-au-lait spots that are flat, light brown, or tan and roughly form an oval shape.
-
Also known as macular stains, these develop before or shortly after birth and are related to the vascular (blood vessel) system. There are several different types:
Angel kisses, which usually appear on the forehead and eyelids.
Stork bites appear on the back of the neck, between the eyebrows on the forehead, or on the eyes’ eyelids. They may fade away as the child grows but often persist into adulthood.
Port-wine stains are flat deep-red or purple birthmarks made up of dilated blood capillaries (small blood vessels). They often appear on the face and are permanent.
Strawberry hemangiomas, composed of small, closely packed blood vessels that grow rapidly and appear anywhere on the body. They usually disappear by age nine.
Cavernous hemangiomas are similar to strawberry hemangiomas but go more deeply into the layers of the skin. A bluish-purple color can often characterize these. They also tend to disappear naturally around school age.
Hair Loss
Also called alopecia
Hereditary hair loss: Millions of men and women have hereditary hair loss. This type of hair loss can often be successfully treated. Everyone loses hair. It is normal to lose about 50-100 hairs every day. If you see bald patches or lots of thinning, you may be experiencing hair loss.
-
There are many causes of hair loss. Women may notice hair loss after giving birth. People under a lot of stress can see noticeable hair loss. Some diseases and medical treatments can cause hair loss.
Luckily, most causes of hair loss can be stopped or treated. Anyone troubled by hair loss should see a dermatologist. These doctors specialize in treating our skin, hair, and nails.
-
The most common cause of hair loss is a medical condition called hereditary hair loss. About 80 million men and women in the United States have this type of hair loss. Other names for this type of hair loss are:
Male-pattern baldness.
Female-pattern baldness.
Androgenetic alopecia.
Hives
Also called Uriticaria
Hives are characterized as itchy red, raised welts (also known as wheals) on the skin's surface that can spread or join together and form larger areas of raised lesions. They are generally triggered by exposure to an allergen or chemical irritant. They tend to appear suddenly and often disappear equally as suddenly.
-
Hives are usually an allergic reaction to food, medicine, or animals. They can also be triggered by sun exposure, stress, excessive perspiration, or other, more serious diseases like lupus. Anyone can get hives. They are harmless and non-contagious. Hives may itch, burn, or sting.
-
They rarely need medical attention as they tend to disappear on their own. However, in persistent cases, your dermatologist may prescribe antihistamines or oral corticosteroids. The best way to prevent hives is to discontinue exposure to allergic irritants.
Hives lasting more than six weeks are known as chronic urticaria or swelling below the skin's surface, angioedema. There are no known causes of angioedema, but it can affect internal organs and require medical attention.Hives lasting more than six weeks are known as chronic urticaria or swelling below the skin's surface, angioedema. There are no known causes of angioedema, but it can affect internal organs and require medical attention.
Eczema
Also called Dermatitis
Eczema is a general term used to describe an inflammation of the skin. In fact, eczema is a series of chronic skin conditions that produce itchy rashes, scaly, dry, and leathery areas; skin redness; or inflammation around blisters. It can be located anywhere on the body but most frequently appears in the creases on the face, arms, and legs. Itchiness is the key characteristic and symptom of eczema. When scratched, the lesions may begin to ooze and get crusted. Over time, painful cracks in the scaly, leathery tissue can form.
Eczema affects people of all races, genders, and ages. It is thought to be hereditary and is not contagious. The cause of eczema remains unknown, but it usually has physical, environmental, or lifestyle triggers. Coming into contact with a trigger, such as wind or an allergy-producing fabric, launches the rash and inflammation. Although it is possible to get eczema only once, most cases are chronic and are characterized by intermittent flare-ups throughout a person's life.
-
Atopic Dermatitis is the most frequent form of eczema and is thought to be caused by the body's immune system's abnormal functioning. It is characterized by itchy, inflamed skin. Atopic dermatitis tends to run in families. About two-thirds of the people who develop this form of eczema do so before the age of one. Atopic dermatitis generally flares up and recedes intermittently throughout the patient's life.
Contact dermatitis is caused when the skin comes into contact with an allergy-producing agent or an irritant, such as chemicals. Finding the triggering allergen is important to treatment and prevention. Allergens can be laundry detergent, cosmetics, jewelry, fabrics, perfume, diapers, poison ivy, or poison sumac.
Dyshidrotic Dermatitis strikes the palms of the hands and soles of the feet. It produces clear, deep blisters that itch and burn. Dyshidrotic dermatitis occurs most frequently during the summer months and in warm climates.
Neurodermatitis, also known as Lichen Simplex Chronicus, this is a chronic skin inflammation caused by a continuous cycle of scratching and itching in response to a localized itch, like a mosquito bite. It creates scaly patches of skin, most commonly on the head, lower legs, wrists, or forearms. Over time, the skin may become thickened and leathery.
Nummular Dermatitis appears as round patches of irritated skin that may be crusted, scaly, and extremely itchy. Nummular dermatitis most frequently appears on the arms, back, buttocks, and lower legs and is usually a chronic condition.
Seborrheic Dermatitis is a common condition that causes yellowish, oily, and scaly patches on the scalp, face, or other body parts. Dandruff, in adults, and cradle cap, in infants, are both forms of seborrheic dermatitis. Unlike other types of eczema, seborrheic dermatitis does not necessarily itch. It tends to run in families. Known triggers include weather, oily skin, emotional stress, and infrequent shampooing.
Stasis Dermatitis, also known as varicose eczema, this form of eczema is a skin irritation that appears on middle-aged and older adults' lower legs. It is related to circulation and vein problems. Symptoms include itching and reddish-brown discoloration of the skin on one or both legs. As the condition progresses, it can lead to blistering, oozing, and skin lesions.
-
For mild cases, over-the-counter topical creams and antihistamines can relieve the itching. A dermatologist will likely prescribe stronger medicine in persistent cases, such as steroid creams, oral steroids (corticosteroids), antibiotic pills, or antifungal creams to treat any potential infection.
The best form of prevention is to identify and remove the trigger. You should also use mild cleansers and keep your skin well moisturized at all times. Also, avoid scratching the rash (which can lead to infection) and situations that make you sweat, such as strenuous exercise.
Melasma
Melasma (muh-LAZ-muh) is a common skin problem. It causes brown to gray-brown patches on the face. Most people get it on their cheeks, bridge of their nose, forehead, chin, and above their upper lip. It also can appear on other parts of the body that get lots of sun, such as the forearms and neck.
-
The forehead is a common place for melasma to appear. Women are far more likely than men to get melasma. It is so common during pregnancy that some people call it the mask of pregnancy. Hormones seem to trigger melasma.
-
One of the most common treatments for melasma is sun protection. This means wearing sunscreen every day and reapplying the sunscreen every 2 hours. Dermatologists also recommend wearing a wide-brimmed hat when you are outside. Sunscreen alone may not give you the protection you need.
Moles
Also called Nevi
Moles are brown or black growths, usually round or oval, that can appear anywhere on the skin. They can be rough or smooth, flat or raised, single or in multiples. They occur when cells responsible for skin pigmentation, known as melanocytes, grow in clusters instead of being spread out across the skin. Generally, moles are less than one-quarter inch in size. Most moles appear by the age of 20, although some moles may appear later in life. Most adults have between 10 and 40 moles. Because they last about 50 years, moles may disappear by themselves over time.
-
Most moles are harmless, but a change in size, shape, color, or texture could indicate a cancerous growth. Moles that have a higher-than-average chance of becoming cancerous include:
Congenital Nevi
Moles present at birth. The larger their size, the greater the risk for developing into skin cancer.
Atypical Dysplastic Nevi
Irregularly shaped moles that are larger than average. They often appear to have dark brown centers with light, uneven borders.
-
People with 50 or more moles are at a greater risk of developing skin cancer.
In some cases, abnormal moles may become painful, itchy, scaly, or bleed. It's important to keep an eye on your moles so that you can catch any changes early. We recommend doing a visual check of your body monthly, including all areas that don't have sun exposure (such as the scalp, armpits, or bottoms of feet).
Use the American Academy of Dermatology's ABCDEs as a guide for assessing whether or not a mole may be becoming cancerous:
Asymmetry: Half a mole does not match the other half in size, shape, or color.
Border: The edges of moles are irregular, scalloped, or poorly defined.
Color: The mole is not the same color throughout.
Diameter: The mole is usually greater than 6 millimeters when diagnosed but may also be smaller.
Evolving: A mole or skin lesion different from the rest or changes in size, shape, or color.
If any of these conditions occur, please make an appointment to see one of our dermatologists right away. The doctor may do a biopsy of the mole to determine if it is or isn't cancerous and/or surgically removes it.
Molluscum
Molluscum Contagiosum
Cantharidin was first isolated from the Spanish Fly by a French chemist in 1810 and has been used as a medicine worldwide. It is nicknamed Beetlejuice.
It is used to treat viral warts and molluscum contagiosum in many dermatology offices as a non-painful and effective treatment. Physicians and practices not adequately trained to use cantharidin should avoid use because it is very safe and painless with training but can lead to painful, devastating blisters if not used correctly. At home, use is NOT recommended.
-
A gel is placed on the bump that causes a blister “bubble” to form on the viral wart or molluscum.
The gel only affects the superficial epidermal cells and does not affect deep skin; therefore, it does not cause scarring but is only a mild treatment for thick warts. It is a great treatment for molluscum.
-
Wash the treated areas with mild soap and water within 2-4 hours
Within 24-48 hours, a blister should form and fall off in the form of a scab.
Advise child not to rub or pick at the area
Typically the area should be well healed in 7 days.
If the area treated was in a “dirty” area like the groin, mouth, or feet, vinegar soaks for 5-10 minutes using 1/3 white vinegar 2/3 water on a clean cloth can help prevent infection.
You do not have to use a bandaid or cover unless the area becomes painful, tender, or unsightly.
The average number of treatments is 3 spread 3-6 weeks apart for molluscum and 4-6 treatments for viral warts.
Nail Disorders
Nail fungus causes changes to the infected nails. You may see white spots or a change in the nail’s color. Other signs include debris under the nail and thickening nails.
-
It’s easy to get a fungal nail infection. If you have a fungal infection on your foot, the fungus can spread to one or more of your nails. This is quite common.
You can also catch a fungal nail infection in a warm, moist place like a pool deck or locker room. If someone else has a fungal infection and walked barefoot there, all you have to do is walk barefoot in the same area. Having wet nails for a long time can also lead to nail fungus. Some people develop it when they wear the same pair of sweaty shoes or boots every day. Fingernails that are wet for hours at a time due to a job or hobby are also susceptible.
What you see on infected nails will vary with the type of fungus causing the infection. Most people see some nail discoloration. The nail may have a white spot. Some nails turn yellow, brown, or green. As the infection worsens, infected nails can thicken, lift from the finger or toe, or crumble. Some nails become thinner.
-
Treatment is important. It can prevent the infection from causing more damage to your nails.
If you have diabetes or a weakened immune system, treatment is essential. After getting a fungal nail infection, people who have diabetes have an increased risk of developing sores that do not heal. Sores that do not heal can lead to serious health problems. It’s important to see a dermatologist (or another doctor) at the first sign of a nail problem. A dermatologist can tell you whether you have a nail infection or something else.
Early diagnosis and treatment are recommended for everyone who has nail fungus. Caught early and treated, a fungal nail infection is likely to clear, and you’ll regrow a healthy nail. Treatment can also prevent the fungus from spreading to other parts of your body and other people.
You cannot get rid of a nail infection by covering it with nail polish or artificial nails.
Psoriasis
Psoriasis is a skin condition that creates red patches of skin with white, flaky scales. It most commonly occurs on the elbows, knees, and trunk but can appear anywhere on the body. The first episode usually strikes between the ages of 15 and 35. It is a chronic condition that will then cycle through flare-ups and remissions throughout the patient's life. Psoriasis affects as many as 7.5 million people in the United States. About 20,000 children under age 10 have been diagnosed with psoriasis.
In normal skin, skin cells live for about 28 days and then are shed from the skin's outermost layer. With psoriasis, the immune system sends a faulty signal, which speeds up the growth cycle. Skin cells mature in a matter of 3 to 6 days. The pace is so rapid that the body cannot shed the dead cells, and patches of raised red skin covered by scaly, white flakes form on the skin.
Psoriasis is a genetic disease (it runs in families) but is not contagious. There is no known cure or method of prevention. Treatment aims to minimize the symptoms and speed healing.
-
There are five distinct types of psoriasis:
Plaque Psoriasis- (Psoriasis Vulgaris) About 80% of all people living with psoriasis get this form of the disease. It is typically found on the elbows, knees, scalp, and lower back. It classically appears as inflamed, red lesions covered by silvery-white scales.
Guttate Psoriasis- This form of psoriasis appears as small red dot-like spots, usually on the trunk or limbs. It occurs most frequently among children and young adults. Guttate psoriasis comes on suddenly, often in response to other health problems or environmental triggers, such as strep throat, tonsillitis, stress, or injury to the skin. Inverse
Psoriasis- This type of psoriasis appears as bright red lesions that are smooth and shiny. It is usually found in the armpits, groin, under the breasts, and in skin folds around the genitals and buttocks.
Pustular Psoriasis- Pustular psoriasis looks like white blisters filled with pus surrounded by red skin. It can appear in a limited area of the skin or all over the body. The pus is made up of white blood cells and is not infectious. Triggers for pustular psoriasis include overexposure to ultraviolet radiation, irritating topical treatments, stress, infections, and sudden withdrawal from systemic (treating the whole body) medications.
Erythrodermic Psoriasis- One of the most inflamed forms of psoriasis, erythrodermic psoriasis looks like fiery, red skin covering large areas the body that shed in white sheets instead of flakes. This form of psoriasis is usually very itchy and may cause some pain. Triggers for erythrodermic psoriasis include severe sunburn, infection, pneumonia, medications, or abrupt withdrawal of systemic psoriasis treatment.
-
People who have psoriasis are at greater risk for contracting other health problems, such as heart disease, inflammatory bowel disease, and diabetes. It has also been linked to a higher incidence of cardiovascular disease, hypertension, cancer, depression, obesity, and other immune-related conditions.
Psoriasis triggers are specific to each person. Some common triggers include stress, injury to the skin, medication allergies, diet, and weather.
-
Psoriasis is classified as Mild to Moderate when it covers 3% to 10% of the body. Mild to moderate psoriasis can generally be treated at home using a combination of three key strategies: over-the-counter medications, prescription topical treatments, and light therapy/phototherapy.
Over-the-Counter Medications
The U.S. Food and Drug Administration has approved two active ingredients for the treatment of psoriasis: salicylic acid, which works by causing the outer layer to shed, and coal tar, which slows the rapid growth of cells. Other over-the-counter treatments include:
Scale lifters that help loosen and remove scales so that medicine can reach the lesions.
Bath solutions, like dilated oatmeal, Epsom salts, or Dead Sea salts, remove scaling and relieve itching.
Occlusion, where topical treatments have been applied, are covered to improve absorption and effectiveness.
Anti-itch preparations, such as calamine lotion or hydrocortisone creams.
Moisturizers are designed to keep the skin lubricated, reduce redness and itchiness, and promote healing.
Prescription Topical Treatments
Prescription topicals focus on slowing down the growth of skin cells and reducing any inflammation. They include:
Anthralin is used to reduce the growth of skin cells associated with plaque.
Calcipotriene that slows cell growth flattens lesions and removes scales. It is also used to treat psoriasis of the scalp and nails.
Calcipotriene and Betamethasone Dipropionate. In addition to slowing down cell growth, flattening lesions, and removing scales, this treatment helps reduce the itch and inflammation associated with psoriasis.
Calcitriol, an active form of vitamin D3 that helps control excessive skin cell production.
Tazarotene, a topical retinoid used to slow cell growth.
Topical steroids, the most commonly prescribed medication for treating psoriasis. Topical steroids fight inflammation and reduce the swelling and redness of lesions.
Light Therapy/Phototherapy
Controlled exposure of skin to ultraviolet light has been a successful treatment for some forms of psoriasis. Three primary light sources are used:
Sunshine, both UVA and UVB rays, can help alleviate psoriasis symptoms but must be used with careful monitoring to ensure that no other skin damage occurs. It is advised that exposure to sunshine be in controlled, short bursts.
Excimer lasers are used to target specific areas of psoriasis. The laser emits a high-intensity beam of UVB directly onto the psoriasis plaque. It generally takes between 4 and 10 treatments to see a tangible improvement.
Pulse dye lasers use a different wavelength of UVB light, similar to the excimer laser. In addition to treating smaller psoriasis areas, it destroys the blood vessels that contribute to the for’ formation. It generally takes about 4 to 6 sessions to clear up a small area with a lesion.
-
Moderate to Severe when it covers more than 10% of the body. The severity of the disease impacts the choice of treatments. Treatments for moderate to severe psoriasis include prescription medications, biologics, and light therapy/phototherapy.
Oral medications
This includes acitretin, cyclosporine, and methotrexate. Your doctor will recommend the best oral medication based on your condition's location, type, and severity.
Biologics
A new classification of injectable drugs, biologics are designed to suppress the immune system. These tend to be very expensive and have many side effects, so they are generally reserved for the most severe cases.
Light Therapy/Phototherapy
Controlled exposure of skin to ultraviolet light has been a successful treatment for some forms of psoriasis. Two primary light sources are used:
Sunshine— both UVA and UVB rays
Sunshine can help alleviate psoriasis symptoms but must be used with careful monitoring to ensure that no other skin damage occurs. It is advised that exposure to sunshine be limited to controlled, short bursts.
PUVA
This treatment combines a photosensitizing drug (psoralens) with UVA light exposure. This treatment takes several weeks to produce the desired result. In some severe cases, phototherapy using UVB light may lead to better results.
Rosacea
Rosacea is a chronic skin condition that causes facial redness, acne-like pimples, visible small blood vessels on the face, swelling, and/or watery, irritated eyes. This inflammation of the face can affect the cheeks, nose, chin, forehead, or eyelids. More than 14 million Americans suffer from rosacea. It is not contagious, but there is some evidence to suggest that it is inherited. There is no known cause or cure for rosacea. There is also no link between rosacea and cancer.
Rosacea generally begins after age 30 and goes through cycles of flare-ups and remissions. Over time, it gets ruddier in color, and small blood vessels (like spider veins) may appear on the face. If left untreated, bumps and pimples may form, the end of the nose may become swollen, red, and bulbous and eyes may water or become irritated.
-
Rosacea occurs most often among people with fair skin who tend to blush or flush easily. It occurs more often among women than men, but men tend to suffer from more severe symptoms. Most patients experience multiple symptoms at varying levels of severity. Common symptoms include:
Flushing
Persistently red skin on the face
Bumps or acne-like pimples
Visible blood vessels on facial skin
Watery or irritated eyes
Burning, itching, or stinging of facial skin
Skin roughness and dryness
Raised red patches
Swelling (edema)
These symptoms may also appear on the neck, chest, scalp, and ears.
-
Research conducted by the National Rosacea Foundation found that the leading triggers for rosacea are:
Sun exposure
Hot or cold weather
Emotional stress
Wind
Alcohol
Heavy exercise
Spicy foods
Hot baths
Heated beverages
Some skincare products
Humidity
Indoor heat
-
While there is no cure for rosacea, and each case is unique, your doctor will probably prescribe oral antibiotics and topical medications to reduce the symptoms' severity. When the condition goes into remission, only topical treatments may be needed. In more severe cases, a vascular laser, intense pulsed light source, or other medical devices may be used to remove any visible blood vessels and reduce excess redness and bumpiness on the nose.
To help reduce the incidence of flare-ups, a gentle daily skin care routine is recommended that includes the use of mild, non-abrasive cleansers, soft cloths, rinsing in lukewarm water (not hot or cold), and blotting the face dry (not rubbing). Additionally, individuals with rosacea need to protect themselves from sun exposure by using sunscreens with SPF 15 or higher and sunblocks that eliminate UVA and UVB rays. Patients are also encouraged to keep a record of flare-ups to try and determine the lifestyle and environmental triggers that aggravate the condition.
Shingles
Also called Herpes Zoster
Shingles is a painful rash that is caused by the varicella-zoster virus. It usually appears as a band or strip of blisters on one side of the body that goes from the spine around the front to the breastbone. However, shingles can also appear on the neck, nose, and forehead.
-
Shingles derive from the same virus that causes chicken pox. After having chicken pox, the virus lies dormant in nerve tissue underneath the skin. Years later, and with no known reason, it reactivates and causes shingles. Shingles are contagious and can easily pass through touching from one person to another. The virus develops into shingles for people who have had chicken pox and develops into chicken pox for those who have not had it. Shingles appear most frequently among older adults (age 60+) and in people with compromised immune systems. Generally, a person only gets shingles once; it rarely recurs.
Symptoms for shingles include:
Pain, burning, numbness, or tingling on one side of the body. The pain often precedes any other symptoms.
A rash that appears a few days after the pain. It may be itchy.
Blisters that break open and then crust over.
Fever, achiness, or headache.
Some people never get a rash or blisters with shingles but experience the pain.
-
Shingles are diagnosed based on a medical history and physical examination of the telltale rash. If you suspect you may have shingles, it is important to contact your doctor as quickly as possible. Early treatment can reduce the pain and severity of the episode. Two types of medications are prescribed to treat shingles:
Antiviral drugs to combat the virus, such as acyclovir, valacyclovir, and famciclovir.
Pain medicines, from oral pain pills and antidepressants to anticonvulsants and topical preparations that contain skin-numbing agents.
Shingles usually heal in about 2 to 3 weeks without any problem. However, a small percentage of patients (10% to 15%), predominantly over age 50, experience pain that lasts beyond one month after the healing period. This is called postherpetic neuralgia. Catching shingles early and beginning treatment can reduce the likelihood and severity of postherpetic neuralgia. See your dermatologist for pain relief.
The U.S. Food and Drug Administration has approved a vaccine, called Zostavax, to prevent adult shingles. It is approved for adults age 60 or older who have had chicken pox. Essentially, the vaccine delivers a booster dose of chicken pox. The vaccine has proven to be very effective in reducing the incidence of shingles and postherpetic neuralgia.
Blue Light Therapy
We can treat acne, precancerous sun spots or scarring due to acne with Blue Light Therapy. Blue Light is a treatment that is non-invasive and effective. It is used to treat acne, actinic keratoses as well as sun-damaged skin. This procedure can be done on the full face and neck.
-
The Blu-U acne light works with all skin types and acts by killing acne-causing bacteria, overactive oil glands, premalignant skin cells and pre-cancers.
Blue Light or Blu-U is a state-of-the-art system in photofacial therapy. The blue light system delivers painless light of blue color that greatly enhances the results of your skin rejuvenation
-
Pre/Post Treatment Instructions can be found here.
Blu-U Light can be paired with IPL for more improvement of brown spots and acne.
Product Recommendations: Gunn Dermatology AOX Mineral Sunscreen and Avene Cicalfate
Vitiligo
Vitiligo refers to the development of white patches anywhere on the skin. With this condition, pigment-forming cells (known as melanocytes) are destroyed by the immune system, causing the skin's loss of pigmentation. Vitiligo usually develops between the ages of 10 and 40. It affects both men and women and appears to be hereditary.
Vitiligo usually affects areas of skin that have been exposed to the sun. It also appears in body folds, near moles, or at the site of previous skin injury. The condition is permanent, and there is no known cure or prevention. However, some treatments can improve the appearance of the skin, such as steroid creams and ultraviolet light therapy.
Rashes
"Rash" is a general term for a wide variety of skin conditions. A rash refers to a change that affects the skin and usually appears as a red patch or small bumps or blisters. The majority of rashes are harmless and can be treated effectively with over-the-counter anti-itch creams, antihistamines, and moisturizing lotions.
-
Rashes can be a symptom of other skin problems. The most prevalent of these are:
Atopic Dermatitis, the most common form of eczema.
Bacterial Infections, such as impetigo.
Contact Dermatitis, a type of eczema caused by coming into contact with an allergen.
Chronic skin problems, such as acne, psoriasis, or seborrheic dermatitis.
Fungal Infections, such as ringworm and yeast infection.
Viral Infections, such as shingles.
-
A rash may signify a more serious illness, such as Lyme Disease, Rocky Mountain Spotted Fever, liver disease, kidney disease, or some types of cancers. If you experience a rash that does not go away on its own after a few weeks, make an appointment to see one of our dermatologists to have it properly diagnosed and treated.
Warts
Warts are small, harmless growths that appear most frequently on the hands and feet. Sometimes they look flat and smooth. Other times, they have a dome-shaped or cauliflower-like appearance. Warts can be surrounded by skin that is either lighter or darker. Warts are caused by different forms of Human Papilloma Virus (HPV). They occur in people of all ages and can spread from person-to-person and from one part of the body to another. Warts are benign (noncancerous) and generally painless. They may disappear without any treatment. However, in most cases eliminating warts takes time. The location of a wart often characterizes its type.
-
Common warts can appear anywhere on the body, although they most often appear on the back of fingers, toes, and knees. These skin-colored, dome-shaped lesions usually grow where the skin has been broken, such as a scratch or bug bite. They can range in size from a pinhead to 10mm and may appear singly or in multiples.
Filiform warts look like a long, narrow, flesh-colored stalk that appears singly or in multiples around the eyelids, face, neck, or lips. They are sometimes called facial warts. They may cause itching or bleeding but are easy to treat with over-the-counter medications.
Flat (plane) warts appear on the face and forehead. They are flesh-colored or white, with a slightly raised, flat surface, and they usually appear in multiples. Flat warts are more common among children and teens than adults.
Genital warts appear around the genital and pubic areas. It is also possible to get genital warts inside the vagina and anal canal or in the mouth (known as oral warts). The lesions start small and soft but can become quite large. They often grow in clusters. They are both sexually transmitted and highly contagious. In fact, it is recommended you generally avoid sex with anyone who has a visible genital wart. A physician should always treat genital warts.
Plantar warts appear on the feet' soles and can be painful since they are on weight-bearing surfaces. They have a rough, cauliflower-like appearance and may have a small black speck in them. They often appear in multiples and may combine into a larger wart called a mosaic wart. Plantar warts can spread rapidly.
Subungual and periungual warts appear as rough growths around the fingernails and/or toenails. They start as nearly undetectable, pin-sized lesions and grow to pea-sized with rough, irregular bumps with uneven borders. Subungual and periungual warts can impede healthy nail growth. Because of their location, they are difficult to treat and generally require medical attention.
-
Most warts respond to over-the-counter treatments, including:
Cryotherapy, which freezes off the wart using liquid nitrogen or nitrous oxide.
Electrosurgery, which sends an electric current through the wart to kill the tissue.
Laser surgery, which essentially heats the wart until the tissue dies and the wart eventually falls off.
Nonprescription freezing products (dimethyl ether), aerosol sprays that freeze warts cause them to die.
Salicylic acid preparations, which dissolve the protein (keratin) that makes up the wart and the thick layer of skin that covers it. It comes in gels, pads, drops, and plasters and takes 4 to 6 weeks to eradicate warts.
If self-treatments don't work after a period of about 4 to 12 weeks, contact our dermatologist. We'll assess your warts and recommend the best option.
Always contact the dermatologist if a wart is causing pain, changes in color or appearance, and all genital warts.
Skin Cancer
IGSRT, or image-guided superficial radiotherapy, is a non-surgical treatment that uses low levels of X-ray energy to kill the cancer cells and allow normal tissue to grow back in its place. It is the only skin cancer treatment with ultrasound imaging, so you and your doctor can see the cancer, precisely target the tumor, and watch it shrink over the course of the treatment. It is delivered in stages, which typically involve 3-5 treatments per week for 4-7 weeks. Each treatment is painless and can be done in as little as 15 minutes. Up to 3 tumors can be treated at one time, and the dose can be adjusted at every stage based on the tumor response.
-
IG-SRT has a cure rate of 99% for basal cell carcinoma and squamous cell carcinoma, making it one of the most effective treatments available for advanced skin cancer based on clinical studies.
-
Unlike Mohs surgery, there is no cutting, bleeding, scarring, or need for reconstructive surgery. You will not need anesthesia. You can continue your normal daily activities during the course of the treatment.